Dr. Shilpa Kshatriya–Nonsustained Ventricular Tachycardia (NSVT)
Nonsustained ventricular tachycardia (NSVT) is defined as 3 or more consecutive beats at a rate of > beats/min and lasting < 30 s.
In some settings, NSVT is a marker of increased risk for subsequent sustained tachyarrhythmias and sudden cardiac death. In other settings they have no prognostic significance. NSVT in the presence of structural heart disease carries a more serious prognosis than in the absence of cardiac abnormality.
SYMPTOMS:
Symptoms of PVCs and NSVT may include palpitations, chest pain, pre-syncope, syncope or heart failure.
GOALS OF TREATMENT IN NSVT:
1.Prevention of malignant, sustained arrhythmias and sudden cardiac death
2.Elimination of symptoms caused by NSVT
SYMPTOM CONTROL:
NSVT is often asymptomatic but some patients experience symptoms such as palpitations, dizziness and dyspnea. Options for treatment include:
- BETA BLOCKERS- safe, well tolerated
- NONDIHYDROPYRIDINE CALCIUM CHANNEL BLOCKERS- can be useful especially in patients who do not have structural heart disease
- ANTIARRHYTHMIC MEDICATIONS-for some patients who have frequent, highly symptomatic NSVT not adequately suppressed by beta blockers or calcium channel blockers, the addition of antiarrhythmic medications may be helpful.
- CATHETER ABLATION-in patients who have very frequent, monomorphic NSVT not controlled by medications or are unable or unwilling to take medications, catheter ablation can be effective in reducing or eliminating NSVT and associated symptoms.
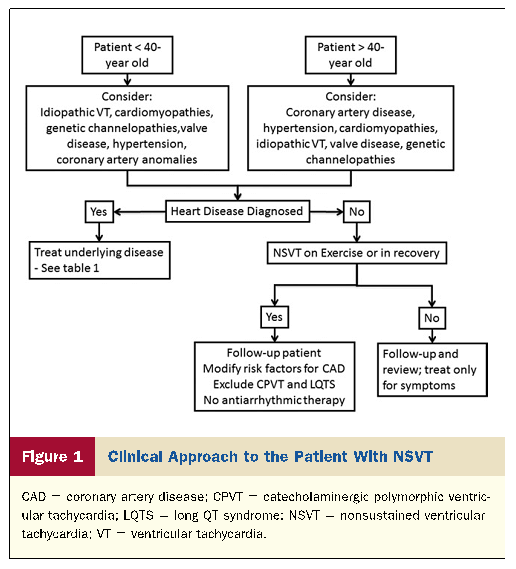
NSVT IN APPARENTLY NORMAL HEART
The following should be considered: age, general condition, previous medical history, history of sudden death and syncopal episodes in family members, and conditions such as electrolyte disturbances, metabolic imbalance, and proarrhythmic effect of drugs should be considered.
In patients > 40 years with episodes of NSVT ischemic heart disease (IHD) should.
Before age 40 years, patients should be evaluated primarily to rule out nonischemic causes of arrhythmia, including hypertension and valve disease, cardiomyopathies, and inherited channelopathies such as long QT syndrome (LQTS), catecholaminergic polymorphic VT, Brugada syndrome, and other early repolarization syndromes that usually present with polymorphic episodes.
When no pathology is identified NSVT needs no specific therapy other than symptom control. However, follow-up is advisable because inherited channelopathies may remain latent for several years.
Idiopathic VT. Monomorphic episodes of NSVT in apparently healthy individuals are often due to idiopathic ventricular outflow arrhythmias.
These tachycardias are adrenergically mediated and sensitive to adenosine or verapamil.
Tachycardias mainly (70% to 80%) arise in the right ventricular outflow tract (RVOT) and rarely below it, and 20% to 30% from the left ventricular outflow tract (LVOT). The tachycardia often occurs during exercise but disappears as the heart rate increases and returns during the recovery period.
RVOT tachycardias produce a left bundle branch block (LBBB) pattern with inferior axis and R/S transition at or beyond V4. LVOT tachycardias may produce a right bundle branch block (RBBB) morphology with inferior axis and R/S transition at V1 or V2.
In symptomatic patients, treatment should be directed toward relief of tachycardia-related symptoms with beta- blockers or calcium-channel blockers and adenosine, if needed in an acute setting. Class IC antiarrhythmic drugs, preferably in combination with beta-blockers may also be tried. If medication is not effective, radiofrequency catheter ablation is recommended and is successful in more than 80% of cases with a low risk of relapse during follow-up .
NSVT IN HYPERTENSION AND VALVE DISEASE
The prognostic value of NSVT in patients with hypertension (without evidence for concomitant IHD) remains unclear. In patients with valvular disease, the inci- dence of NSVT is considerable (up to 25% in aortic stenosis and in significant mitral regurgitation) and appears to be a marker of underlying LV pathology. Presence of NSVT is usually associated with LV hypertrophy or dysfunction, but no convincing evidence exists to prove that NSVT is an independent predictor of sudden death in patients with valve disease.
Aggressive treatment of hypertension (including beta blockers) is the therapy of choice in patients with hypertension and NSVT.
CORONARY ARTERY DISEASE
Non–ST-segment elevation acute coronary syndromes.
In non–ST-segment elevation acute coronary syndromes, NSVT is detected in 18% to 25% of patients 2 to 9 days after admission.The coexistence of NSVT with myocardial ischemia indicates 10% risk of sudden death, with most episodes occurring within the first 3 months after the documentation of NSVT and ischemia.
Myocardial infarction. In acute MI, NSVT during the first 24 hours is frequent (45% in patients without thrombolysis and up to 75% in reperfused patients). Following the first 7 days after MI, NSVT is detected in approximately 6.8% to 13.4%. Monomorphic NSVT suggests re-entry at the borders of a ventricular scar due to previous MI, whereas ischemia most of the time induces polymorphic NSVT/VF.
Clinical assessment of ischemic patients with NSVT.
It is important to perform an ischemic evaluation. Acute myocardial ischemia is an established cause of polymorphic ventricular rhythms. Ischemia may induce sustained or nonsustained monomorphic VT in the presence of a myocardial scar.
Echocardiography may detect signs of cardiomyopathy or other structural abnormalities and impaired LV function. Holter monitoring is a valuable diagnostic tool for detecting patients with NSVT.The major utility of electrophysiologic (EPS) testing in patients with NSVT and IHD is in those with LVEF between 30% and 40%. In NSVT in the context of reduced LVEF (<40%), inducibility of sustained monomorphic VT at baseline EPS is associated with a 2-year risk of sudden death or cardiac arrest of 50% compared with a 6% risk in patients without inducible VT .
Therapy of ischemic patients with NSVT.The treatment of ischemic patients with NSVT should first include therapy for IHD, such as revascularization, beta- blockers, statins, and angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors.
LV Dysfunction and Heart Failure
In patients with ischemic and nonischemic heart failure and LVEF < 30% to 40%, the rprevalence of NSVT is 30% to 80%. In dilated cardiomyopathy, NSVT has been detected in 40% to 50% of patients. The most useful risk stratifier is LVEF and recommendations for ICD are mainly based on LVEF and symptomatic status of heart failure i.e NYHA functional class.
Hypertrophic Cardiomyopathy (HCM)
There is no characteristic ECG morphology of NSVT in patients with HCM. Up to 20% to 30% of patients may have NSVT, whereas this proportion approaches 80% in patients with a history of cardiac arrest. NSVT confers an increased risk for sudden cardiac death in hypertrophic cardiomyopathy.
Beta-blockers may decrease the risk of sudden death, but defibrillator implantation is the therapy of choice in the presence of high-risk factors, including frequent NSVT accompanied by history of syncope or family history of sudden death at young age.
The Major Risk Factors for Sudden Cardiac Death (SCD)in HCM patients:
- H/o cardiac arrest
- Spontaneous sustained ventricular tachycardia
- Family h/o premature SCD
- Unexplained syncope
- LV thickness ≥ 30mm
- Abnormal bp response (hypotensive) to exercise
- NSVT
Arrhythmogenic Right Ventricular Cardiomyopathy
The tachycardias in ARVC arise from the right ventricle and typically present with LBBB morphology with a left or even right axis deviation.
ICD seems to be the therapy of choice in patients with cardiac arrest, syncope, or hemodynamically poorly tolerated VT despite antiarrhythmic therapy.
Conclusions
NSVT can be present in apparently healthy individuals as well as those with significant heart disease. Prognosis depends on the underlying condition, and in several clinical settings is not known. The management of patients with NSVT is aimed at treating the underlying heart disease rather than the arrhythmia itself, unless serious symptoms occur.